New technology revolutionizes heart transplants
At 24 years old, Danielle Perea was newly enrolled in a clinical lab science master's program, living with her boyfriend in Louisiana, and generally enjoying her life — until one day, a stomachache led to her sitting in an area hospital, being told she had just hours left to live.
Just a few days into her program, Perea woke with a "serious stomachache" that she first mistook for food poisoning, but when she used the bathroom she passed "frothy blood" that made her decide to go to the emergency room at a hospital she did not name because of pending litigation. Perea was told that a CT scan taken by doctors showed no signs of a problem.
When her symptoms persisted, she went to another hospital where she was observed again, but still not diagnosed with anything. Doctors looked at the same CT scan, and said something like a clot was unlikely because of her age and relative health. On the third day of her symptoms, Perea began vomiting blood, and again returned to the emergency room as her symptoms intensified.
An exploratory surgery revealed that there had been a blood clot in one of the vessels that carries blood from the small intestines, a condition called mesenteric ischemia. Surgeons attempted to salvage the organs, but found too much necrotic tissue.
"They just saw that everything was completely black, necrotic, dead," Perea told CBS News. "They (told my boyfriend) 'There's no way she's going to survive this, you need to call her parents. Get anyone here who needs to be here, because she probably has 24 hours to live.'"

Perea went into hospice care, but exceeded expectations, maintaining "strong vitals" for over a week. During that time, her mother and boyfriend searched for a miracle. They learned about Cleveland Clinic's intestinal transplant program, the largest in the nation, and the head of the program, Dr. Kareem Abu-Elmagd, agreed to take Perea's case.
What is an intestinal transplant, and why are they so rare?
An intestinal transplant replaces the small intestine with a new organ. Just 95 were conducted in the United States last year, according to Dr. Masato Fujiki, director of intestinal transplantation at Cleveland Clinic and one of the doctors who treated Perea. Eighteen of those were done at the Cleveland Clinic, making it the largest intestinal transplant program in the country. During the same time period, there were over 10,000 liver transplants and more than 4,000 heart transplants.
There are about 15,000 eligible organ donors each year, and there are not many patients eligible for an intestinal transplant. This allows doctors to "be very selective, to get the best organ," Fujiki said. Ideal intestinal donors are people who are under the age of 50 and in good health, and who have stable blood pressure.
While it's not particularly difficult to find a suitable organ, intestinal transplants did not have a high success rate until recently, contributing to their rarity, Fujiki said. Intestines are a "difficult" organ to monitor, he said, and intestinal transplants have the highest rejection rate of any kind of organ transplant.
The one-year graft survival rate for a patient who has an intestinal transplant was up to 82% in 2022, from a rate of 76.2% in 2018, according to national data. That's still below the graft survival rate for more common procedures like liver transplants, which have a rate of 85 to 90%, Fujiki said.
An extended road to recovery
Once Perea's family learned about the intestinal transplant program and her case had been accepted at Cleveland Clinic, she was brought to the Ohio hospital. Her small bowel was almost entirely resected. Her condition was stabilized, and after several other procedures, she was officially added to the transplant list in the spring of 2019.
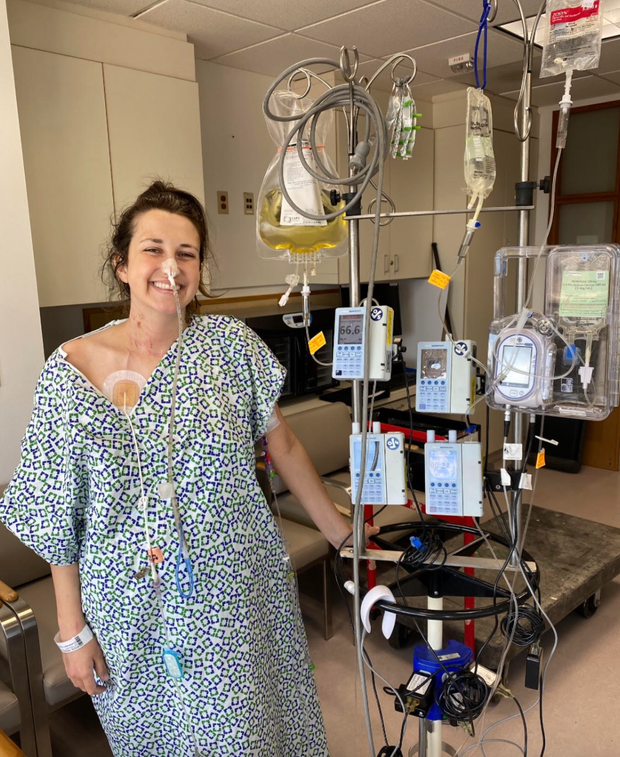
Before the transplant, Perea spent a year and a half living on IV-administered nutrition because without the intestines, she couldn't eat normally. The amount of time she spent being supported by machines meant Perea had to have another surgery to repair damage to her trachea before she could receive the transplant, extending the amount of time she had to wait. The coronavirus pandemic also complicated the process, forcing her to pass on an organ in April 2020.
Finally, in June 2020, Perea got the call she had been waiting for.
"They were just like, 'You need to get to the clinic right away.' It wasn't an option," Perea said.
The surgery took 10 hours, and even once the new organ was in place, Perea continued to spend time in the hospital, being readmitted for frequent fevers. In January 2021, she had another procedure to repair her abdominal wall and reverse her ileostomy, an incision made during the surgery.
Now, four years after the operation, she told CBS News that she can live relatively normally, though she does take "about 40 pills a day." There is the possibility she might need a kidney transplant in the future, because of the impact of anti-rejection medications on that organ, and she has annual appointments at the Cleveland Clinic to monitor the transplant, but everything has been "super normal" so far.
"I don't have any restrictions. My incisions healed well. I got married in November," Perea said. "We bought a house. It's just all going well."
At Cleveland Clinic, she said, "they're like, 'Just keep living your life. There's nothing stopping you.'"

Kerry Breen is a news editor at CBSNews.com. A graduate of New York University's Arthur L. Carter School of Journalism, she previously worked at NBC News' TODAY Digital. She covers current events, breaking news and issues including substance use.
